The Causes Of Posterior Tibial Tendon Dysfunction ?
Overview
Chronic posterior tibial tendon insufficiency can result in acquired adult flatfoot deformity. This is a chronic foot condition where the soft-tissues (including the posterior tibial tendon, deltoid and spring ligaments) on the inside aspect of the ankle are subject to repetitive load during walking and standing. Over time these structures may become painful and swollen ultimately failing. When these supporting structures fail the result is a change in the alignment of the foot. This condition is typically associated with a progressive flatfoot deformity. This type of deformity leads to increased strain on the supporting structures on the inside of the ankle and loading through the outer aspect of the ankle and hind-foot. Both the inside and outside of the ankle can become painful resulting significant disability. This condition can often be treated without surgery by strengthening the involved muscles and tendons and by bracing the ankle. When non-operative treatment fails, surgery can improve the alignment replace the injured tendon. Alignment and function can be restored, however, the time to maximal improvement is typically six months but, can take up to a year. 
Causes
Several risk factors are associated with PTT dysfunction, including high blood pressure, obesity, diabetes, previous ankle surgery or trauma and exposure to steroids. A person who suspects that they are suffering from PTT dysfunction should seek medical attention earlier rather than later. It is much easier to treat early and avoid a collapsed arch than it is to repair one. When the pain first happens and there is no significant flatfoot deformity, initial treatments include rest, oral anti-inflammatory medications and, depending on the severity, a special boot or brace.
Symptoms
Depending on the cause of the flatfoot, a patient may experience one or more of the different symptoms here. Pain along the course of the posterior tibial tendon which lies on the inside of the foot and ankle. This can be associated with swelling on the inside of the ankle. Pain that is worse with activity. High intensity or impact activities, such as running, can be very difficult. Some patients can have difficulty walking or even standing for long periods of time. When the foot collapses, the heel bone may shift position and put pressure on the outside ankle bone (fibula). This can cause pain on the outside of the ankle. Arthritis in the heel also causes this same type of pain. Patients with an old injury or arthritis in the middle of the foot can have painful, bony bumps on the top and inside of the foot. These make shoewear very difficult. Occasionally, the bony spurs are so large that they pinch the nerves which can result in numbness and tingling on the top of the foot and into the toes. Diabetics may only notice swelling or a large bump on the bottom of the foot. Because their sensation is affected, people with diabetes may not have any pain. The large bump can cause skin problems and an ulcer (a sore that does not heal) may develop if proper diabetic shoewear is not used.
Diagnosis
Your podiatrist is very familiar with tendons that have just about had enough, and will likely be able to diagnose this condition by performing a physical exam of your foot. He or she will probably examine the area visually and by feel, will inquire about your medical history (including past pain or injuries), and may also observe your feet as you walk. You may also be asked to attempt standing on your toes. This may be done by having you lift your ?good? foot (the one without the complaining tendon) off the ground, standing only on your problem foot. (You may be instructed to place your hands against the wall to help with balance.) Then, your podiatrist will ask you to try to go up on your toes on the bad foot. If you have difficulty doing so, it may indicate a problem with your posterior tibial tendon. Some imaging technology may be used to diagnose this condition, although it?s more likely the doctor will rely primarily on a physical exam. However, he or she may order scans such as an MRI or CT scan to look at your foot?s interior, and X-rays might also be helpful in a diagnosis.
Non surgical Treatment
Because of the progressive nature of PTTD, early treatment is advised. If treated early enough, your symptoms may resolve without the need for surgery and progression of your condition can be arrested. In contrast, untreated PTTD could leave you with an extremely flat foot, painful arthritis in the foot and ankle, and increasing limitations on walking, running, or other activities. In many cases of PTTD, treatment can begin with non-surgical approaches that may include orthotic devices or bracing. To give your arch the support it needs, your foot and ankle surgeon may provide you with an ankle brace or a custom orthotic device that fits into the shoe. Immobilization. Sometimes a short-leg cast or boot is worn to immobilize the foot and allow the tendon to heal, or you may need to completely avoid all weight-bearing for a while. Physical therapy. Ultrasound therapy and exercises may help rehabilitate the tendon and muscle following immobilization. Medications. Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, help reduce the pain and inflammation. Shoe modifications. Your foot and ankle surgeon may advise changes to make with your shoes and may provide special inserts designed to improve arch support. 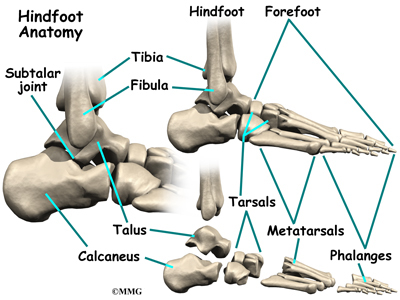
Surgical Treatment
The indications for surgery are persistent pain and/or significant deformity. Sometimes the foot just feels weak and the assessment of deformity is best done by a foot and ankle specialist. If surgery is appropriate, a combination of soft tissue and bony procedures may be considered to correct alignment and support the medial arch, taking strain off failing ligaments. Depending upon the tissues involved and extent of deformity, the foot and ankle specialist will determine the necessary combination of procedures. Surgical procedures may include a medial slide calcaneal osteotomy to correct position of the heel, a lateral column lengthening to correct position in the midfoot and a medial cuneiform osteotomy or first metatarsal-tarsal fusion to correct elevation of the medial forefoot. The posterior tibial tendon may be reconstructed with a tendon transfer. In severe cases (stage III), the reconstruction may include fusion of the hind foot,, resulting in stiffness of the hind foot but the desired pain relief. In the most severe stage (stage IV), the deltoid ligament on the inside of the ankle fails, resulting in the deformity in the ankle. This deformity over time can result in arthritis in the ankle.